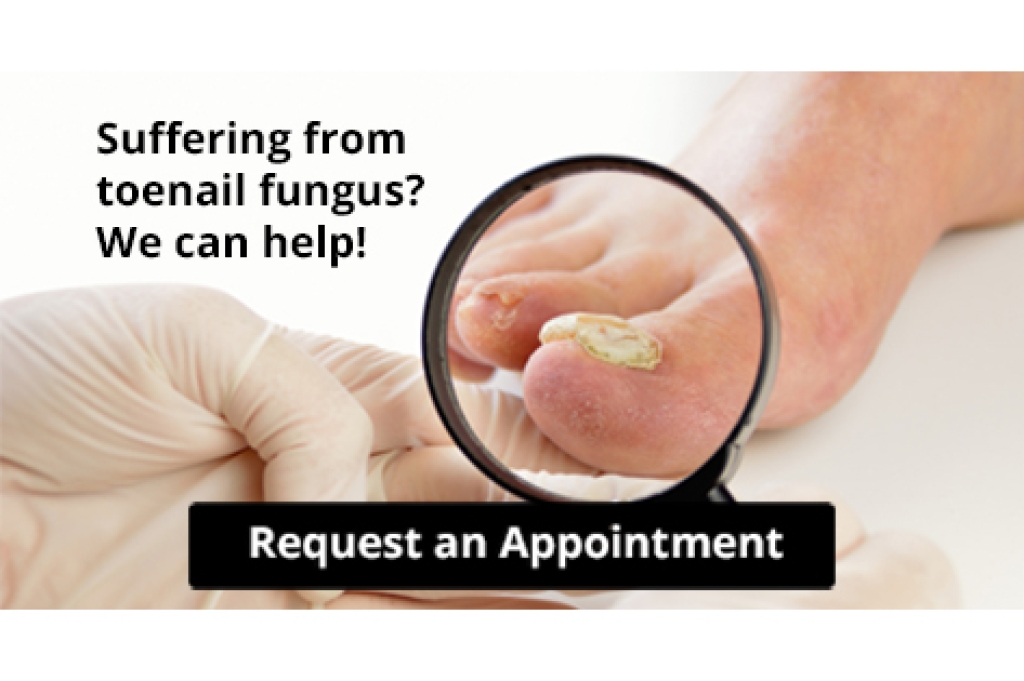
Athlete's foot, a prevalent fungal infection, predominantly affects the feet, with the skin between the toes being especially vulnerable. Athlete's foot is caused by various fungi, with the most common being trichophyton, which thrives in warm, humid environments. Athlete’s foot infections result in a moist, itchy, red, or flaky rash between the toes. Other symptoms are cracked, scaly, or peeling skin and stinging and burning sensations on cracked skin. Itchy blisters that form may burst and leave scales, and result in a dry, scaly rash on the soles and up the sides of the foot. If left untreated, athlete's foot can progress to more severe stages, with symptoms such as bleeding from cracked skin and white, soggy skin in toe webbing. An unpleasant odor, oozing blisters, and pain in affected areas can occur. Thickened, crumbly, or discolored toenails may develop if the fungus spreads. Transmission occurs through contaminated floors in shared spaces like showers and changing rooms, as well as in socks, clothing, and used towels. Prevention involves practicing good foot hygiene, wearing well-ventilated shoes, and avoiding walking barefoot in communal areas. For a severe case of athlete’s foot, it is suggested that you schedule an appointment with a podiatrist for advanced treatment.
Athlete’s foot is an inconvenient condition that can be easily reduced with the proper treatment. If you have any concerns about your feet and ankles, contact David Carmack, DPM from Texas. Our doctor will treat your foot and ankle needs.
Athlete’s Foot: The Sole Story
Athlete's foot, also known as tinea pedis, can be an extremely contagious foot infection. It is commonly contracted in public changing areas and bathrooms, dormitory style living quarters, around locker rooms and public swimming pools, or anywhere your feet often come into contact with other people.
Solutions to Combat Athlete’s Foot
- Hydrate your feet by using lotion
- Exfoliate
- Buff off nails
- Use of anti-fungal products
- Examine your feet and visit your doctor if any suspicious blisters or cuts develop
Athlete’s foot can cause many irritating symptoms such as dry and flaking skin, itching, and redness. Some more severe symptoms can include bleeding and cracked skin, intense itching and burning, and even pain when walking. In the worst cases, Athlete’s foot can cause blistering as well. Speak to your podiatrist for a better understanding of the different causes of Athlete’s foot, as well as help in determining which treatment options are best for you.
If you have any questions please feel free to contact our office located in Marble Falls, TX . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.